Annual Report 2017/18 Strategy, policy and research
What's on this page
Our strategy Communication and engagement Strategy and research Multi-profession policyOur strategy
AHPRA and the National Boards are working to a five-year strategy: the National Registration and Accreditation Scheme strategy 2015–20. The information contained in this report shows how we are performing in relation to our statutory obligations, as well as how we are tracking against our strategy.
Our mission
To protect the public by regulating health practitioners efficiently and effectively to facilitate access to safer healthcare.
Our vision
We are recognised as a leading risk-based regulator enabling a competent and flexible health workforce to meet the current and future needs of the Australian community.
Strategic outcomes by 2020
- Reduce risk of harm to the public associated with the practice of regulated health professions.
- Ensure that only health practitioners who are suitably trained and qualified to practise in a competent and ethical manner are registered.
- Increase public confidence in the effective and efficient regulation of health practitioners.
- Increase public benefit from our data for practitioner regulation, health workforce planning and research.
- Improve access to healthcare through our contribution to a more sustainable health workforce.
For more information, visit the National Registration and Accreditation Scheme Strategy page on the AHPRA website.
Refining our strategy for the future
A new strategy and service delivery governance model was implemented in January 2018. The streamlined model prioritises the work we need to do to deliver our strategy, including operating model changes and regulatory reforms.
Our regulatory principles
Eight Regulatory principles underpin our work and guide our decision-making in the public interest. These principles foster a responsive, risk-based approach to regulation. Here are the principles.
- Protect the public
- Take timely and necessary action
- Administer the National Law
- Ensure registrants are qualified
- Work with stakeholders
- Uphold professional standards
- Identify and respond to risk
- Use appropriate regulatory force
Read more about our Regulatory principles on the AHPRA website.
Communication and engagement
Performance snapshot
- 54 newsletters were issued
- The median open rate for newsletters was 67.0%
- We received and responded to 451 media enquiries
- 48 media releases were issued
- 64 court and tribunal summaries were published
- 46.4% increase in Facebook followers
- 19.7% increase in Twitter followers
- 124.9% increase in LinkedIn followers
Media relations
We continue to explain the National Scheme and our processes and share what we can while meeting our confidentiality obligations. This year, we continued our proactive approach to media relations. We received and responded to 451 media enquiries and published 48 media releases and 569 news items across the AHPRA and National Board websites. We published 109 communiqués on the AHPRA and National Board websites after meetings of Boards and some advisory groups, outlining the topics that were discussed.
We also published 64 court and tribunal summaries which outline each matter and its outcome. The summaries provide an important educational opportunity for registered practitioners about acceptable and unacceptable standards of practice and behaviour, and for patients about what they should expect from their practitioner.
Social media
Our social media channels grew considerably this year, with a 46.4%, 19.7% and 124.9% growth on Facebook, Twitter and LinkedIn respectively.
Publications
A total of 54 newsletters were emailed this year, including National Board newsletters that are sent to all registered practitioners and the AHPRA report, which is sent to AHPRA's stakeholders. The newsletters include important information, such as changes to the standards health practitioners need to meet or how regulation is implemented.
AHPRA and the National Boards successfully met the statutory reporting requirement by tabling the 2016/17 annual report in the required timeframe. As at 30 June 2018, the report was downloaded 3,753 times from the AHPRA website.
Seeking feedback
We regularly consult with two advisory groups to gather feedback, information and advice on our work.
Our Community Reference Group (CRG) acts as a 'critical friend' to ensure that we consider the needs and expectations of the community. This year we sought their advice on how to improve the notifier experience, how we can use research to better inform our decision-making, and how we can share work with other government agencies more effectively.
Our Professions Reference Group (PRG) provides an important profession voice in our work. Consisting of one representative from a professional association for each of the regulated professions and one representative from the Health Professions Accreditation Collaborative Forum, they provide advice on a range of operational issues. This year they provided feedback on the changes to the National Law, as well as our work to improve AHPRA processes.
Both groups publish communiques after each meeting for transparency. For CRG meetings, visit the Community Reference Group page on the AHPRA website. For PRG meetings, visit the Professions Reference Group page on the AHPRA website.
Closing the gap
This year, AHPRA and the National Boards developed a commitment by 37 health entities to help achieve equity in health outcomes between Aboriginal and Torres Strait Islander Peoples and other Australians to close the gap by 2031.
The National Scheme Aboriginal and Torres Strait Islander health strategy statement of intent is signed by leading Aboriginal and Torres Strait Islander health organisations, AHPRA, all National Boards and all accreditation authorities.
It was developed in close partnership with a range of Aboriginal and Torres Strait Islander organisations and experts, including the Lowitja Institute, Australian Indigenous Doctors' Association (AIDA), Congress of Aboriginal and Torres Strait Islander Nurses and Midwives (CATSINaM) and National Aboriginal Community Controlled Health Organisation (NACCHO).
The group shares a commitment to ensuring that Aboriginal and Torres Strait Islander Peoples have access to health services that are culturally safe and free from racism so that they can enjoy a healthy life, equal to that of other Australians, enriched by a strong living culture, dignity and justice.
To help achieve this, the group is focused on:
- developing a culturally safe health workforce supported by nationally consistent standards, codes and guidelines across all professions in the National Scheme
- using leadership and influence to achieve reciprocal goals
- increased Aboriginal and Torres Strait Islander Peoples' participation in the registered health workforce
- greater access for Aboriginal and Torres Strait Islander Peoples to culturally safe services of health professions regulated under the National Scheme, and
- increased participation across all levels of the National Scheme.
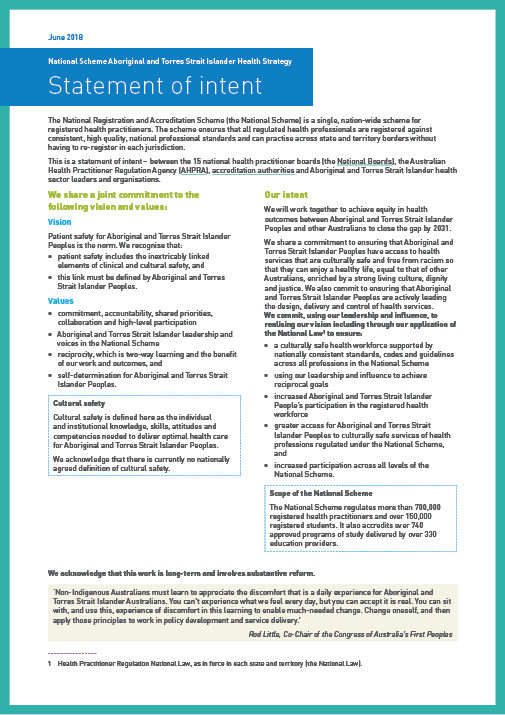
Download the National Scheme Aboriginal and Torres Strait Islander health strategy statement of intent.
Supporting this work: AHPRA's first Reconciliation action plan
This year, AHPRA's first Reconciliation action plan (RAP) was formally endorsed by Reconciliation Australia. This important document outlines what AHPRA will do to support the vision outlined in the National Scheme Aboriginal and Torres Strait Islander health strategy statement of intent and start addressing the imbalance in health outcomes between Aboriginal and Torres Strait Islander Peoples and other Australians.
To read more about the Aboriginal and Torres Strait Islander health strategy group, the National Scheme Aboriginal and Torres Strait Islander health strategy statement of intent or AHPRA RAP, go to the Aboriginal and Torres Strait Islander Health Strategy page on the AHPRA website.

The cover of AHPRA's RAP (artwork by Paul Green)
![Ms Sally Cunningham, Mr Gilbert Hennequin, Dr Ailsa Wood, Ms Jill Humphreys, Ms Narelle Mills, Ms Anita Rivera, Mr Martin Fletcher, Ms Eliza Collier, Mr Michael Piu, Dr Sabine Hammond, Ms Kym Ayscough, Ms Tania Dalton, Mr Michael Gorton, Mr Craig Dukes, Mr Allan Groth; [L–R seated]: Mr Chris Robertson, Mr Karl Briscoe, Ms Jacqui Gibson-Roos, Dr Joanna Flynn, Associate Professor Gregory Phillips, Professor Roianne West, Ms Tanja Hirvonen](assets/img/ATSI-health-strategy-group.jpg)
Attendees at the Aboriginal and Torres Strait Islander health strategy group meeting in March 2018
[L–R standing]: Ms Sally Cunningham, Mr Gilbert Hennequin, Dr Ailsa Wood, Ms Jill Humphreys, Ms Narelle Mills, Ms Anita Rivera, Mr Martin Fletcher, Ms Eliza Collier, Mr Michael Piu, Dr Sabine Hammond, Ms Kym Ayscough, Ms Tania Dalton, Mr Michael Gorton AM, Mr Craig Dukes, Mr Allan Groth; [L–R seated]: Mr Chris Robertson, Mr Karl Briscoe, Ms Jacqui Gibson-Roos, Dr Joanna Flynn AM, Associate Professor Gregory Phillips, Professor Roianne West, Ms Tanja Hirvonen
Strategy and research
AHPRA's strategy and research team supports and facilitates the implementation of our corporate strategy. The team also provides research and evaluation of the regulatory data collected by the National Scheme as well as some external data sources.
The team is responsible for delivering and facilitating continuous improvement of a framework for best practice in implementing strategy, supporting improvement of strategic decision-making, and providing guidance on how to execute scheme strategy with all entities in the National Scheme.
Regulatory planning
Supported by AHPRA's strategy and research team, each of the 15 National Boards carries out annual planning to develop regulatory initiatives in its functions under the National Law, and in alignment with AHPRA's strategic objectives. Whenever possible, these initiatives are consolidated into a multi-profession, scheme-wide approach.
Health Profession Agreements
Under the National Law, each year AHPRA must enter into a Health Profession Agreement with each National Board, which outlines the services provided by AHPRA to the Board, the Board's regulatory plan, and the budget and fees charged to practitioners for the coming year. To find out more, visit the Health profession agreements page on the AHPRA website.
Regulatory research
Within the strategy and research team, the AHPRA research unit has a specific objective to conduct research and evaluation projects to develop evidence-based inputs to assist decision-making and policy development. The unit provides expert advice and guidance in framing research questions and designing studies to meet objectives as well as building capacity for research activities across the Scheme.
Access to research
When our data and information are used for research purposes, they are often published as research outcomes in academic journals and publications. In 2017/18, we started making a list of published research available on the AHPRA website where data and/or information from AHPRA and the National Boards have been used by researchers.
Where publications can be accessed freely by the public, links to external websites are provided on the What data are available page on the AHPRA website.
Research partnerships
The research unit maintains and facilitates formal strategic data and research partnerships, including a National Health and Medical Research Council (NHMRC) partnership grant with the University of Melbourne, who have been investigating hotspots of risk using regulatory data collected by the National Scheme. In the 2017/18 financial year, a number of publications resulted from the partnership, including:
- Ryan, A, Too, LS, and Bismark, M (2018) 'Complaints about chiropractors, osteopaths, and physiotherapists: a retrospective cohort study of health, performance, and conduct concerns', Chiropractic & Manual Therapies 26(12).
- Thomas, LA, Milligan, E, Tibble, HM, and others (2018) 'Health, performance and conduct concerns among older doctors: A retrospective cohort study of notifications received by medical regulators in Australia', Journal of Patient Safety and Risk Management 23(2), 54–62.
- Thomas, LA, Tibble, HM, Too, LS, and others (2018) 'Complaints about dental practitioners: an analysis of 6 years of complaints about dentists, dental prosthetists, oral health therapists, dental therapists and dental hygienists in Australia', Australian Dental Journal [Epub ahead of print].
- Tibble, HM, Broughton, NS, Studdert, DM, and others (2017) 'Why do surgeons receive more complaints than their physician peers?', ANZ Journal of Surgery [E-pub ahead of print].
Policy development
The research unit supports National Boards and other entities across the scheme with research and evaluation activities, including investigating relevant regulatory data about registered practitioners to support the development of regulatory policy, standards, codes and guidelines and regulatory decision-making. In 2017/18, this work included:
- an analysis of notifications involving the supply of pseudoephedrine, which was commissioned by the Pharmacy Board of Australia
- environmental scanning and surveillance of emerging literature monitoring cross-professional trends in risk-based regulation, including managing a service for boards and staff requiring access to journal articles or grey literature
- conducting a number of literature reviews, including the review of relevant academic and grey literature, to obtain up-to-date knowledge of best-practice approaches to inform the review of the current shared code of conduct and the CPD standard
- analysis of data from a survey of pharmacy interns and preceptors to identify factors relating to the quality of supervision provided by preceptors to interns
- completing a comprehensive research report, including a literature review and a notification analysis, to support the Chinese Medicine Board of Australia in establishing a risk-profile for the profession, and
- continuing a cross-professional study assessing the effectiveness of regulatory interventions over a five-year timeframe.
Commissioned research
In 2017, AHPRA commissioned a piece of work in line with its commitment to the Senate Community Affairs Reference Committee inquiry into the medical complaints process in Australia, which had recommended that AHPRA develop and publish a framework for identifying and dealing with vexatious complaints.
The research report 'Reducing, identifying and managing vexatious complaints: Summary report of a literature review prepared for the Australian Health Practitioner Regulation Agency' [Bismark, M, Canaway, R and Morris, J (2017), Centre for Health Policy] was released in April 2018. It takes a first international look at vexatious complaints, finding there is greater risk from people not reporting concerns than from those making truly vexatious complaints. The report outlines a number of principles that will be used to inform best practice for preventing, identifying, and managing vexatious complaints in the future. Visit the What data are available page on the AHPRA website.
Health workforce survey
Each year at renewal, a survey is completed by registered health practitioners to collect critical demographic information about Australia's health practitioner workforce. This year, 96.2% of practitioners responded to the survey as part of the registration renewal process. Over the past year, AHPRA has continued to liaise with the Department of Health (DoH) to facilitate the secure and timely transfer of survey data and to resolve any issues with data quality.
In 2017/18, DoH published workforce data analyses for all professions regulated by the National Scheme, including profession-specific fact sheets and high-level workforce summaries. You can find the workforce data obtained from the survey on the Australian Government's Health Workforce Data website.
A new framework for our regulatory research
In 2017/18, the research framework for the National Scheme was finalised and published on the Data not publicly available page on the AHPRA website. The framework is designed as a living document that will be regularly updated. It sets out the research priorities and principles for National Boards and AHPRA to focus their research efforts and guide the use of National Scheme data and information to inform policy and decision-making. AHPRA has written to the National Health and Medical Research Council (NHMRC) to share the publication of the research framework and to explore the opportunities for dialogue with the NHMRC about promoting awareness and uptake of the framework.
Implementing our strategy
AHPRA employs the balanced scorecard (BSC) methodology as our strategic framework to enable efficient communication of the National Scheme's vision, mission and strategic outcomes.
Four strategic performance reports have been completed to review our progress in implementing our strategy and measuring its execution. These reports provide a cumulative picture of our strategic performance and will continue to be refined as part of the approach to this first year of reporting. Visit the National Registration and Accreditation Scheme Strategy page on the AHPRA website.
Our strategy builds on a firm foundation of capability and culture in the organisation, which strengthens risk-based regulation, strategic partnerships and service excellence.
Read Figure 18 from the bottom up. Once achieved, each of the objectives described in this map will deliver our vision (to be recognised as a leading risk-based regulator) through our mission (safer healthcare for all Australians).
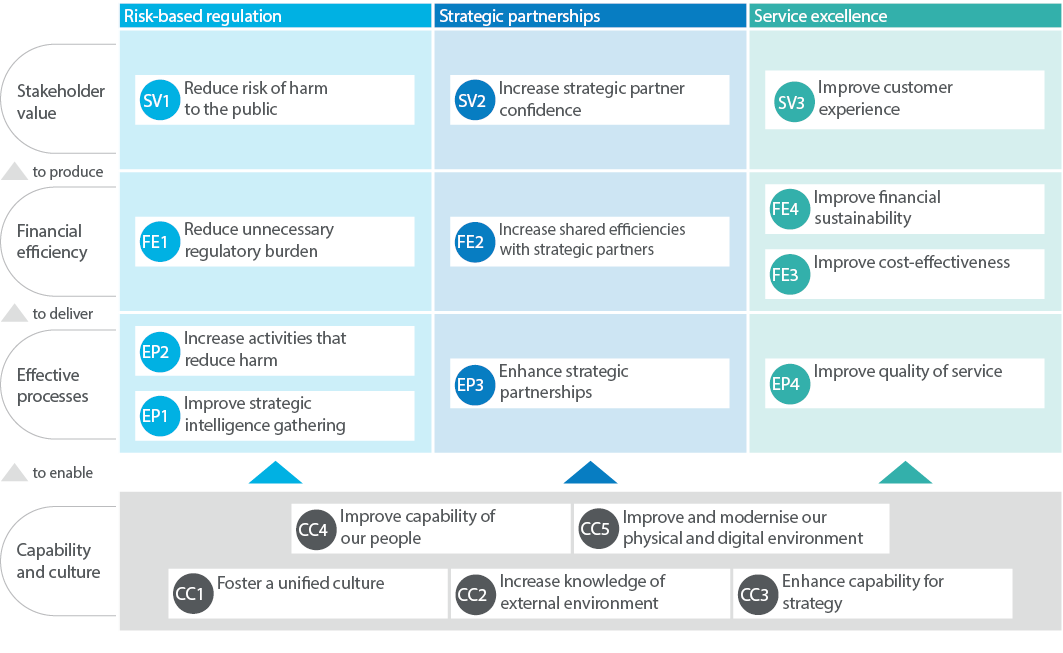
Open an accessible version of Figure 18.
Multi-profession policy
Overview
National Boards regularly collaborate on shared policy issues, where the issue involves the same or similar impacts across professions. Maximising consistency in the regulatory framework across professions facilitates effective collaborative care and supports good practice. It has benefits for consumers and employers by simplifying the regulatory landscape and helping clarify expectations of all registered health practitioners.
Shared policy issues include:
- developing or reviewing common or shared registration standards, codes and guidelines across National Boards
- coordinating reviews of registration standards and guidelines which involve a mix of multi-profession and profession-specific issues
- developing coordinated policy responses to key issues such as advertising
- developing policy resources and tools, and
- coordinating joint submissions to relevant external consultations.
Common registration standards and guidelines have the same content for all National Boards and include the Criminal history registration standard, Guidelines for advertising regulated health services and Guidelines for mandatory notifications.
Shared standards and guidelines have very similar content across National Boards and include the English language skills registration standards for 12 National Boards1 and the Code of conduct shared by seven National Boards and used by an additional five with minor profession-specific variations.
Joint policy initiatives
In 2017/18, we continued substantial work on advertising policy issues, including further implementing the Advertising compliance and enforcement strategy for the National Boards and AHPRA. We developed and published new tools, including self-assessment and testimonials tools, to support the strategy and help practitioners understand their obligations and facilitate compliance and substantially progressed the joint review of the Guidelines for advertising regulated health services. We developed a framework for evaluating the strategy and started data collection.
We completed the final stages of coordinating a joint review of continuing professional development (CPD), recency of practice (ROP) and professional indemnity insurance (PII) registration standards for three National Boards (Aboriginal and Torres Strait Islander Health Practice, Chinese medicine and Occupational therapy), and for Chiropractic and Optometry (CPD only) and Psychology (PII only).
We continued work on a joint review of the Code of conduct shared by seven National Boards and used by an additional five with minor profession-specific variations (Aboriginal and Torres Strait Islander Health Practice, Chinese medicine, Chiropractic, Dental, Medical radiation practice, Occupational therapy, Optometry, Osteopathy, Paramedicine, Pharmacy, Physiotherapy and Podiatry).
We continued work to review the supervised practice guidelines used by a number of National Boards and to establish a clearer, simpler regulatory framework for supervised practice where it is used in registration and notification functions (other than supervision in the context of internships). We tested the proposed framework with stakeholders in preparation for public consultation in 2018/19.
We continued work on the policy framework for scheduled medicines endorsements (visit the Endorsement for scheduled medicines page on the AHPRA website), including implementing additional guidance for National Boards developing a submission to Ministerial Council for approval of endorsement for scheduled medicines.
The inaugural meeting of our Scheduled Medicines Expert Committee (visit the Scheduled Medicine Expert Committee page on the AHPRA website) was held on 27 July 2017 and the committee also met on 1 September 2017, 1 December 2017 and 18 May 2018.
Policy support and coordination
AHPRA's multi-profession policy team develops policy resources and tools to provide policy advice to National Boards. It also develops and coordinates responses for external policy consultations. In 2017/18 examples included:
- Draft therapeutic goods advertising code and associated guidelines
- Victorian Child Safety and Wellbeing Information Sharing consultation
- Commonwealth Department of Employment's update of the Short-term skilled occupation list and Medium and long-term strategic skills list
- Therapeutic Goods Administration consultation on prescription opioid use for pain relief
- Migrant and Women's Health Partnership consultation on the Draft competency standards framework – Culturally responsive clinical practice: Working with people from migrant and refugee backgrounds
- Therapeutic Goods Administration consultation on the proposed model for complaints handling, and
- NSW Parliamentary inquiry into cosmetic health clinics.
What's next?
A focus for 2018/19 will be completing the evaluation of the Advertising compliance and enforcement strategy and the joint reviews of the shared Code of conduct and Guidelines for advertising regulated health services, implementing the core registration standards reviewed by six National Boards subject to Ministerial Council approval and undertaking the first phase of the next review of English language skills registration standards. We will also continue the multi-profession review of limited registration standards, review our Policy manual (a reference for policy staff working with National Boards), coordinate a review of National Boards social media policy and build our behavioural insights resources and capacity.
1 The Nursing and Midwifery Board of Australia's English language skills registration standard has some profession-specific differences to reflect the characteristics of the nursing and midwifery professions; the Paramedicine Board of Australia's English language skills registration standard has some minor differences related to the grandparenting arrangements; and the Aboriginal and Torres Strait Islander Health Practice Board of Australia has a different standard reflecting the unique characteristics of this profession.