Annual Report 2017/18 Performance and overview
What's on this page
About us Introduction Agency Management Committee and National Boards Health practitioner regulation in Australia Highlights The National Scheme in each state and territoryPerformance summary
Registration
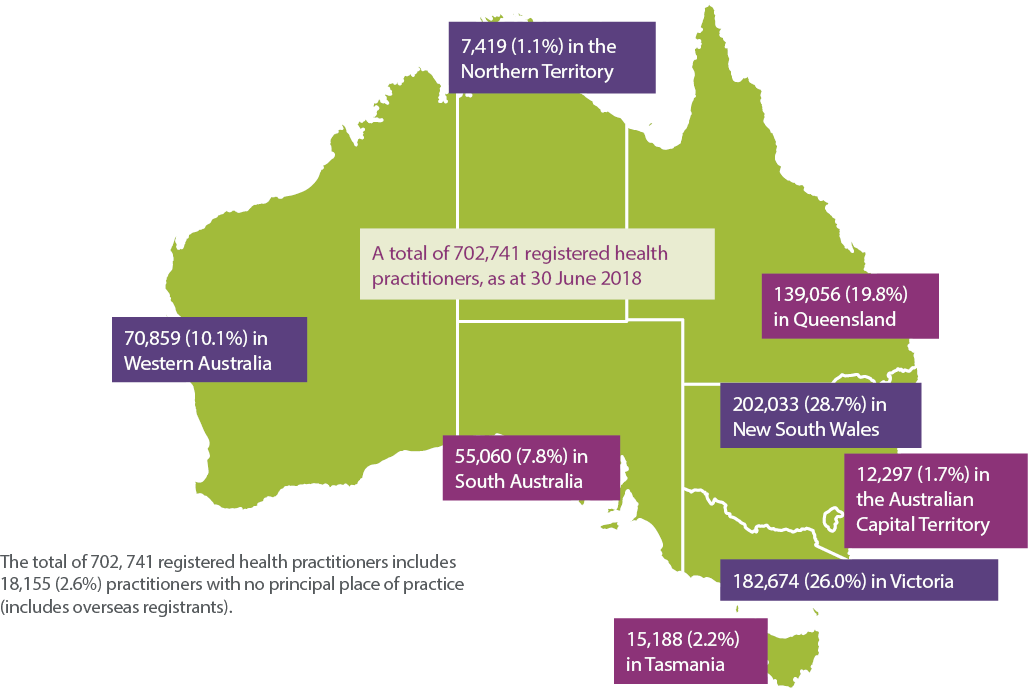
702,741 registered health practitioners in Australia, across 15 professions1
5,953 health practitioners identify as Aboriginal and/or Torres Strait Islander
Over 23,800 (3.5%) more registrants than last year
In May, the number of registered health practitioners in Australia reached 700,000
78,407 domestic and international criminal history checks made
As a result one registration was refused
161,114 students studying to be health practitioners through an approved program of study or clinical training program
99% of registrants renewed and completed their registration online
73,759 new applications for registration received: 6.9% increase since last year 3,401 applications for registration refused because they did not meet suitability/eligibility requirements (4.6% of all new applications)
AHPRA: supporting the National Boards
372,616 calls made to AHPRA's customer service team Average of 1,433 phone calls each day, with up to 5,000 calls a day in peak times 94.2% of telephone enquiries resolved at first contact
86% of health practitioners responded with 'very satisfied' when asked to rate their interaction with our customer service team
53,797 web enquiries received An average of 206 web enquiries each day
630 appointments made comprising: 45 Ministerial appointments of National Board members 115 Ministerial appointments of state and territory board members 242 National Board appointments of national committees, and 228 National Board appointments for state, territory or regional committee membership
Notifications
10,934 practitioners had a notification raised about them nationally, this is an increase of 3.7% from 2016/172
1.6% of all registered health practitioners were the subject of a notification2
The top three reasons for a notification were: clinical care (41.0%) medication-related issues (12.6%) health impairment (8.9%)
Immediate action was taken to restrict or suspend the registration of a practitioner 413 times3
7,276 notifications were received by AHPRA about practitioners2
5.5% increase in notifications received by AHPRA
24.5% of health, performance and conduct matters resulted in regulatory action
97.0% of matters decided nationally by tribunals this year resulted in regulatory action
7.2% increase in mandatory notifications4 received by AHPRA
Appeals
28 appeals lodged in tribunals about Board decisions made under the National Law
Of the 71 appeals that were finalised:
13 resulted in no change to the Board's decision
13 resulted in the decision being amended or substituted for a new decision
36 resulted in the appeal being withdrawn
9 were dismissed on administrative grounds
Statutory offences
1,043 advertising-related complaints received
14 new offence complaints related to restricted practices
18 closed following investigation
416 new offence complaints received relating to title protection
485 closed following investigation
12 cases of falsely claiming to be a registered health practitioner successfully prosecuted before the courts
Accreditation
The National Scheme accredits over 740 approved programs of study delivered by over 330 education providers
Compliance
2,752 practitioners were monitored by AHPRA for health, performance and/or conduct during the year
Notes:
- In 2017/18, 14 National Boards regulated 15 professions. The Nursing and Midwifery Board of Australia regulates two professions – nursing and midwifery.
- Includes data provided by the Health Professional Councils Authority (HPCA) for New South Wales (NSW) and the Office of the Health Ombudsman (OHO) for Queensland (based on available data from these entities at time of publication).
- This refers to notifications managed by AHPRA (excludes data from HPCA and OHO). For information on how complaints about health practitioners are lodged and managed in Australia, see page below.
- Notification that an entity is required to make to AHPRA under Division 2 of Part 8 of the Health Practitioner Regulation National Law (the National Law). Refer to the Glossary for more definitions.
About us
The Australian Health Practitioner Regulation Agency (AHPRA) is the national organisation responsible for implementing the National Registration and Accreditation Scheme (the National Scheme) across Australia.
AHPRA works in partnership with the National Boards to ensure the community has access to a safe health workforce across all professions currently registered under the National Scheme. Together, we protect the public by regulating health professionals who practise in Australia. Public safety is always our number one priority. Every decision we make is guided by the Health Practitioner Regulation National Law (the National Law), as in force in each state and territory.
What we do
AHPRA delivers five core regulatory functions:
- Professional standards – We provide policy advice to the National Boards about registration standards, codes and guidelines for health practitioners.
- Registration – In partnership with the National Boards, we ensure that only health practitioners with the skills and qualifications to provide competent and ethical care are registered to practise.
- Notifications – We manage complaints and concerns raised about the health, performance and conduct of individual health practitioners.
- Compliance – We monitor and audit registered health practitioners to make sure they are complying with Board requirements.
- Accreditation – We work with accreditation authorities and committees to ensure graduating students are suitably qualified and skilled to apply to register as a health practitioner.
Protecting the public
- We support the National Boards in their primary role of protecting the public.
- We support the National Boards in the development of registration standards, codes and guidelines.
- We publish a national Register of practitioners so that important information about individual health practitioners is available to the public
- We manage registration and renewal processes for local and overseas-qualified health practitioners, and manage student registration.
- We manage notifications about the professional conduct, performance or health of registered health practitioners on behalf of the National Boards, except in New South Wales (NSW) where notifications are managed by health professional councils and the Health Care Complaints Commission (HCCC). In Queensland, we manage notifications referred to us by the Office of the Health Ombudsman (OHO). See page below for more information on health regulation in Australia.
- We work with health complaints entities (HCEs) to make sure the appropriate organisation deals with the community's concerns about health practitioners.
- We provide advice to the Ministerial Council about the administration of the National Scheme.
Due to rounding (to one decimal place), percentages may not add up exactly to 100%.
Supplementary data tables are available online and are the source for some of the statistics cited in this report.
Introduction
AHPRA works collaboratively with the National Boards to implement the work of the National Registration and Accreditation Scheme (National Scheme). At its heart, the National Scheme is about protecting patients and the broader public.
2017/18 was a year of milestones. In May 2018, the number of registered health practitioners in Australia reached 700,000 – the community now has access to more registered practitioners than ever before. Currently, there are over 160,000 registered students working towards entering the registered health workforce.
This year we also welcomed the Paramedicine Board of Australia to the National Scheme. The Board consulted on and finalised Australia's first national registration standards for the profession, communicating extensively with paramedics and their employers to prepare them for regulation under the National Scheme. This will be the first time paramedics have been registered in Australia.
Another national first was the development and launch of a shared commitment between Aboriginal and Torres Strait Islander health leaders, AHPRA, the National Boards and accreditation authorities. The National Scheme Aboriginal and Torres Strait Islander health strategy statement of intent is a commitment to achieve equity in health outcomes between Aboriginal and Torres Strait Islander Peoples and other Australians to close the gap by 2031.
We were honoured to be designated a World Health Organization (WHO) Collaborating Centre for health workforce regulation across the Western Pacific. This designation means that we will work with WHO and countries in the Western Pacific to strengthen regulatory practice across the region and to learn from the best of international experience for our work in Australia. This is an important focus in an era of increased global mobility for both health practitioners and patients.
In our eighth year of operations, we continued to improve our services so that people who engage with us have the information they need. A key component of this work involved inviting feedback from practitioners who have been the subject of a notification and people who have lodged notifications, to better understand their experience and how we can support, communicate with and inform both practitioners and notifiers through the process. This is an important ongoing focus for us.
Future arrangements for accreditation have also been a central focus over the past year. During 2017/18, AHPRA worked with National Boards to contribute to the independent Accreditation systems review, including developing submissions to the draft report in October 2017. The final report and Ministers' responses will set the future direction for accreditation in the National Scheme.
We have worked hard to ensure collaborative relationships with stakeholders including through our Community Reference Group, our Professions Reference Group and with our co-regulatory partners.
At the core of the National Scheme is the partnership between AHPRA and the National Boards. The Chairs of the National Boards, along with the Agency Management Committee Chair and senior AHPRA staff meet quarterly as the Forum of National Registration and Accreditation Scheme Chairs. This Forum provides a unique opportunity for discussion of common issues facing the National Scheme. Dr Joanna Flynn AM co-convened the Forum with Mr Michael Gorton AM until May 2018. Mr Ian Bluntish, Chair of the Optometry Board of Australia, has now taken over from Dr Flynn as Forum Co-convenor.
The Australian community places great trust in registered health practitioners. We are committed to ensuring that the National Scheme registers and regulates practitioners efficiently and effectively to facilitate access to safer healthcare for all Australians.

Mr Martin Fletcher
Chief Executive Officer, AHPRA

Mr Michael Gorton AM
Co-convenor, Forum of National Registration and Accreditation Scheme Chairs
Chair, Agency Management Committee, AHPRA

Dr Joanna Flynn AM
Co-convenor, Forum of National Registration and Accreditation Scheme Chairs (until May 2018)
Chair, Medical Board of Australia

Mr Ian Bluntish
Co-convenor, Forum of National Registration and Accreditation Scheme Chairs (from May 2018)
Chair, Optometry Board of Australia
Agency Management Committee and National Boards
The Agency Management Committee is appointed by the Ministerial Council to oversee AHPRA's work.
In 2017/18, the Agency Management Committee members were:
- Mr Michael Gorton AM, (Chair)
- Adjunct Professor Karen Crawshaw PSM
- Mr Ian Smith PSM
- Ms Jenny Taing
- Ms Barbara Yeoh AM
- Dr Peggy Brown AO
- Dr Susan Young
- Ms Philippa Smith AM.
For more information, visit the Agency Management Committee page on the AHPRA website.
The National Executive is the national leadership group within AHPRA. In 2017/18 its members were:
- Mr Martin Fletcher, Chief Executive Officer
- Ms Sarndrah Horsfall, Executive Director, Business Services
- Ms Kym Ayscough, Executive Director, Regulatory Operations
- Mr Chris Robertson, Executive Director, Strategy and Policy
- Ms Judith Pettitt, Interim Executive Director, People and Culture (March–June 2018).
The National Boards are responsible for the regulation of health professions, setting registration standards, codes, guidelines and policies that all health practitioners must meet in order to be registered.
The National Boards are:
- Aboriginal and Torres Strait Islander Health Practice Board of Australia
- Chinese Medicine Board of Australia
- Chiropractic Board of Australia
- Dental Board of Australia
- Medical Board of Australia
- Medical Radiation Practice Board of Australia
- Nursing and Midwifery Board of Australia1
- Occupational Therapy Board of Australia
- Optometry Board of Australia
- Osteopathy Board of Australia
- Paramedicine Board of Australia2
- Pharmacy Board of Australia
- Physiotherapy Board of Australia
- Podiatry Board of Australia, and
- Psychology Board of Australia.
National Board members are appointed by the Ministerial Council.
AHPRA has a Health Profession Agreement with each National Board which are published on the Health profession agreements page on the AHPRA website. For more information on who we are and how AHPRA and the National Boards work together, please visit the About AHPRA page on the AHPRA website.
All Board websites are accessible via AHPRA's homepage.
1 The Nursing and Midwifery Board of Australia regulates two professions – nursing and midwifery.
2 The Paramedicine Board of Australia was established in October 2017 and is preparing for the regulation of paramedics, which is expected to begin in late 2018.

Health practitioner regulation in Australia
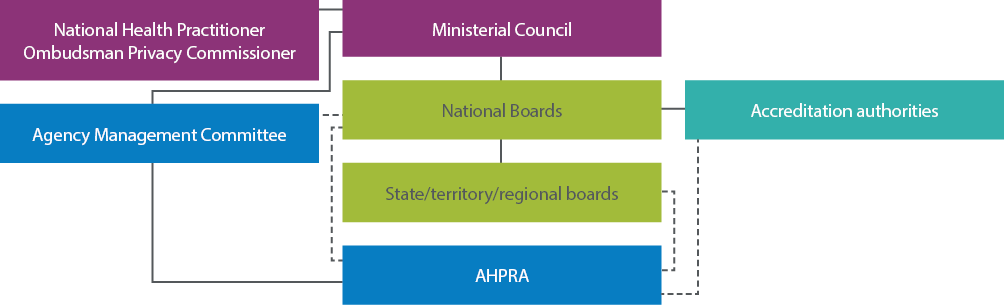
The National Law provides a regulatory framework for the accreditation and registration of health practitioners (see Figure 1). While this law is nationally consistent, two states have also adopted a co-regulatory approach. So, where does AHPRA fit in?
AHPRA and the National Boards work in a dynamic regulatory environment. We are responsible for the registration of every practitioner in the registered health professions across Australia. However, the regulation of these practitioners is a shared responsibility.
If someone wants to make a complaint or raise a concern about a registered health practitioner in most states and territories in Australia, they can visit our complaints portal. However, if their complaint is about a registered health practitioner or student in New South Wales (NSW) or Queensland, the process is different.
New South Wales
The National Boards and AHPRA do not manage notifications that arise in NSW.
Fourteen health professional councils – supported by the Health Professional Councils Authority (HPCA) and working with the Health Care Complaints Commission (HCCC) – work together to assess and manage complaints about practitioners' conduct, health and performance in NSW.
The National Boards have no role in handling notifications in NSW. AHPRA has a limited role in accepting mandatory notifications and referring them to the HCCC.
AHPRA ensures that all NSW notifications and their outcomes are recorded to ensure the national register is accurate and complete.
For more information about the notifications process in NSW, visit the HPCA website or the HCCC website.
Queensland
The National Boards and AHPRA only manage complaints that arise in Queensland if the Office of the Health Ombudsman (OHO) refers the complaints to us.
OHO receives all complaints that arise in Queensland. It may refer a complaint to AHPRA and the National Boards if OHO is satisfied that the complaint is not serious.
For more information about the notifications process in Queensland, visit the OHO website.
Other health complaint organisations
Under the National Law, AHPRA and the National Boards work with health complaints entities (HCEs) in each state and territory to decide which organisation should take responsibility for, and manage, a complaint or concern raised about a registered health practitioner. HCEs also handle complaints about unregistered health practitioners, and can provide outcomes that AHPRA and the National Boards cannot, such as:
- an apology or explanation
- access to your health records
- compensation or a refund, and/or
- an improvement for a hospital, clinic, pharmacy or community health service.
Following is a list of HCEs in each state and territory:
- Australian Capital Territory – ACT Human Rights Commission
- New South Wales – Health Care Complaints Commission
- Northern Territory – Health and Community Services Complaints Commission
- Queensland – Office of the Health Ombudsman
- South Australia – Health and Community Services Complaints Commission
- Tasmania – Health Complaints Commissioner
- Victoria – Health Complaints Commissioner, and
- Western Australia – Health and Disability Services Complaints Office.
Anyone needing advice on how to make a complaint can call AHPRA's customer service team on 1300 419 495 or visit the Make a notification page on the AHPRA website for information.
Highlights
Reaching 700,000 registered practitioners
Health practitioner registration is core to what we do, although it often draws less attention than any regulatory action taken.
In May, with the registration of an enrolled nurse in Victoria, the number of registered health practitioners in Australia reached 700,000.
This milestone comes almost eight years after the launch of the National Scheme, when AHPRA and the National Boards began their regulatory partnership. It demonstrates the success of that partnership as an enabler of the Australian health workforce to deliver health services to communities across the country.
Strengthening international collaboration
AHPRA and the National Boards continued their commitment to best practice and learning from others.
In November 2017, AHPRA and the National Boards co-hosted the International Congress on Professional and Occupational Regulation with the Council on Licensure, Enforcement and Regulation (CLEAR). The event successfully provided a forum for over 200 regulators from across the world, and from a wide range of sectors, to meet, share and learn about best practice regulation to better protect the public.
In December 2017, AHPRA was designated a World Health Organization Collaborating Centre for health workforce regulation across the Western Pacific. Part of this work will be to strengthen regulatory practice across the region, including establishing a network of health workforce regulators across Southeast Asia and the Western Pacific to improve regulatory standards.
Improving consumer access to public information
Changes to the national online register aim to improve access to information about registered health practitioners.
In March 2018, following the recommendations from the independent review of the use of chaperone conditions, the Medical Board of Australia updated the Register of practitioners, including links to disciplinary decisions by courts and tribunals when there was an adverse finding about a doctor.
The register helps consumers know more about the registered health practitioners they may choose to seek care from. It is an important way in which the National Scheme helps keep the public safe.
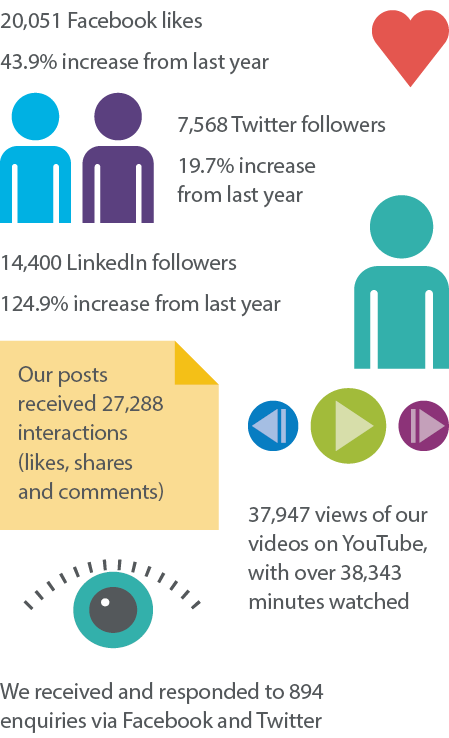
Engaging with the community
At its heart, practitioner regulation aims to work in the best interests of the community. That is why AHPRA and the National Boards aim for strong community engagement through AHPRA's Community Reference Group (CRG).
The CRG is made up of members of the broader community who work to ensure that the community's voice is heard about strategies for improving knowledge and awareness of health practitioner regulation in the community.
The CRG provides AHPRA with feedback and input on the work we do, and the services we deliver. The group's function is to provide advice on a range of matters that affect consumers. It consistently calls for the consumer perspective to be included in aspects of the work of the National Scheme.
Importantly, members have provided valuable feedback on the journey for notifiers, which has helped inform AHPRA's ongoing national program of work on improving the experience for both practitioners and notifiers. During the year, the CRG also provided input into consultations that will shape health practitioner regulation, including on the Accreditation systems review, the revised Nursing and Midwifery Board codes of conduct launched in March 2018, and the development of the Aboriginal and Torres Strait Islander health strategy statement of intent.
Delivering customer service
Providing timely information for patients, health consumers and health practitioners is a primary concern for AHPRA's customer service team (CST).
Our goal is to answer 70% of all calls within 90 seconds and online enquiries within 48 hours.
In 2017, the CST was consolidated into one location, launching in Sydney on 1 July. Centralising the team has allowed for improvements and greater consistency in service delivery and training for staff. It also means that we can better manage and plan for the demands put on the CST during peak registration and renewal periods.
In 2017/18, we received up to 1,639 calls and online enquiries per day, with close to 5,000 calls a day during peak times. We improved our overall online services performance by 6.3% and calls to our contact centre reduced by 7.3%. This year we responded to online enquiries in an average of 25.21 hours, well within 48 hours.
We rolled out our most successful renewal campaign to date for nurses and midwives. This campaign is the biggest and busiest campaign of the year. During the campaign the CST improved its performance by 22.6% in call services and 23% in online services response rate.
Achieving advertising compliance
AHPRA and the National Boards have helped advertisers of regulated health services stay within the law through a new strategy focused on education and compliance.
Our risk-based approach to advertising compliance and enforcement recognises that most health practitioners want to comply with the law. It is supported by a strong education focus. Indications are that our strategy of educating practitioners and working closely with stakeholders to support better understanding of the legal requirements is working. When advised that their advertising does not comply with the National Law, practitioners are generally making the necessary corrections without the need for further action. Published resources, including a self-assessment tool, are helping practitioners check and correct their advertising.
Investing time to educate practitioners and engaging with professional associations is effective. Part of this is due to the strategy creating an environment that supports voluntary compliance and builds community confidence in regulation. You can read more on the Legislation guidelines page on the AHPRA website.
Working to improve the National Scheme
AHPRA is committed to continual improvement and an important way that we can do this is by listening to feedback that we receive. Feedback is always welcome at AHPRA, whether good or bad, as it allows us to ensure our service is improved for everybody.
The National Health Practitioner Ombudsman and Privacy Commissioner (NHPOPC) is an important part of the National Scheme. The NHPOPC was established by Health Ministers to coincide with the introduction of the National Law. It provides an independent ombudsman, privacy and freedom of information oversight of the National Scheme, particularly in relation to the work that AHPRA and the National Boards do and the administrative processes experienced by practitioners and the public. NHPOPC's work helps to improve the services we provide.
We meet regularly with the Ombudsman to receive feedback and recommendations. This collaborative relationship means we are better able to respond swiftly to feedback and improve our services and complaint-handling processes.
Online improvements
Technology improvements are making it easier to engage with us online.
Our new online portal helped smooth the path to registration for the more than 25,600 graduates who applied by April 2018 without needing to provide hardcopy forms. As well as making the process easier for applicants, the portal also enhances the identity-check component of an application by linking directly with the Australian government agencies who issue key identity documents. The addition of an application tracker means graduates can monitor the progress of AHPRA's assessment of their registration application. You can find out more on the Graduate Applications page on the AHPRA website.
The National Scheme in each state and territory
The National Scheme operates Australia-wide and is a vital part of the Australian health system. It is governed by a nationally consistent law passed by each state and territory parliament – the National Law. There is oversight by a Ministerial Council made up of all Australia's Health Ministers.
The National Scheme facilitates the regulation of individual health practitioners, not health services themselves. Health practitioners are also expected to meet the requirements of other parts of the health system within which they operate, whether a local hospital, health authority, government department or statutory authority.
Above all else, the National Scheme is in place to protect patients. It builds consistent and local decision-making supported by national standards. This is supported by local AHPRA offices in each capital city, which manage stakeholder engagement and work with boards and committees at a local level.
Figure 2 shows the number of registered health practitioners in each state and territory in Australia and each state and territory's percentage of the total number of practitioners.